Part III: National Infrastructure (ABDM)
Digital Health at Scale: The NHA Perspective
A critical highlight from Himanshu Burad (NHA) involves the deployment of digital health solutions across India's diverse landscape. Contrary to common myths about rural digital literacy, India is demonstrating that digital health can be adopted at a staggering scale.
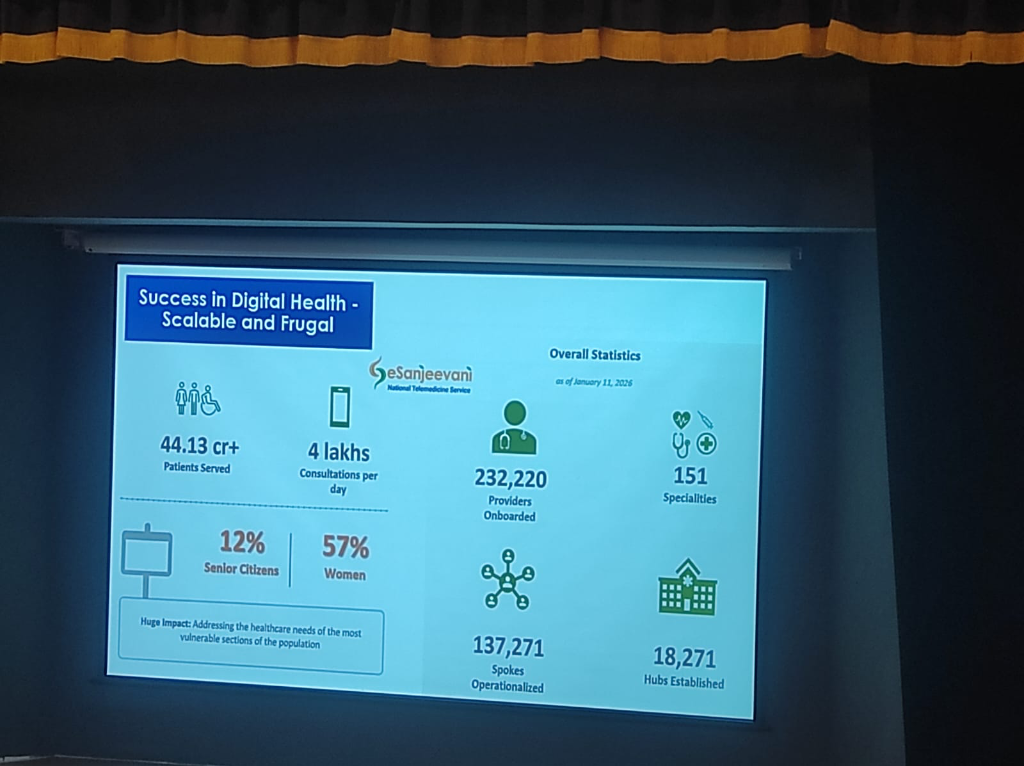 Figure: The scale of E-Sanjeevani as of January 11, 2026.
Figure: The scale of E-Sanjeevani as of January 11, 2026.
- E-Sanjeevani: Telemedicine for the Millions: Launched in 2018, the E-Sanjeevani platform has transformed healthcare access in rural areas.
- Total Patients Served: Over 44.13 Crore (441 Million).
- Daily Velocity: Currently averaging 4 Lakh (400,000) consultations per day.
- Provider Network: 232,220 providers onboarded across 151 specialities.
- Infrastructure Footprint:
- Hubs Established: 18,271 specialist hubs.
- Spokes Operationalized: 137,271 peripheral units.
- Inclusivity & Demographics: The platform is successfully addressing the needs of underserved populations:
- Women: Account for 57% of the total beneficiaries.
- Senior Citizens: Represent 12% of the user base.
- Rural Empowerment: These numbers illustrate that the rural population—connected through sub-health centers to specialists in district hospitals—is actively and effectively utilizing digital health solutions.
- The Economic Impact: Telemedicine is not just a clinical tool; it is an economic stabilizer for the rural poor.
- Time Savings: Patients save an average of 18 hours of time per consultation by avoiding travel and long hospital wait times.
- Wage Protection: For a daily wage laborer, a trip to a specialist in a city often consumes a full day. Accessing care via E-Sanjeevani saves one full day of daily wages, ensuring that seeking health doesn't lead to financial instability.
- CoWIN: Digital Orchestration at Staggering Scale:
- Beyond telemedicine, the CoWIN platform stands as a global benchmark for digital health operations.
- At its peak, the system facilitated more vaccinations in a single day than the entire populations of many countries combined. This massive orchestration proved that India's digital public infrastructure can handle load and complexity at a level previously thought impossible across such a vast geography.
India's Digital Foundation: The Internet Journey
The success of these platforms is underpinned by the massive expansion of digital connectivity across the subcontinent.
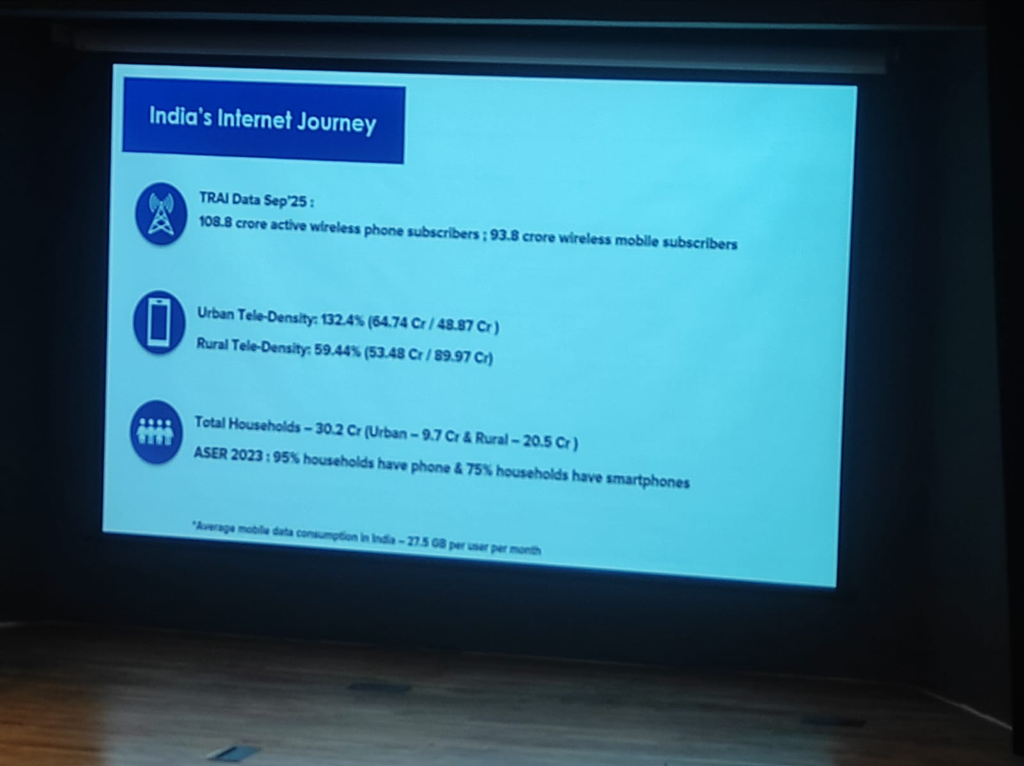 Figure: The growth of mobile and data penetration in India (Source: TRAI/ASER).
Figure: The growth of mobile and data penetration in India (Source: TRAI/ASER).
- The Connectivity Boom: As of September 2025, India has 108.8 Crore active wireless phone subscribers, with 93.8 Crore being mobile data users.
- Rural vs. Urban Tele-Density:
- Urban: 132.4% tele-density.
- Rural: 59.44% tele-density, indicating a significant yet growing footprint in the most remote areas.
- Household Penetration: 95% of the 30.2 Crore households in India have a phone, and 75% already have a smartphone.
-
Data Dominance: India remains a global leader in data consumption, with an average of 27.5 GB per user per month.
-
Champions in Rural Areas: Overcoming digital literacy and infrastructure challenges in rural regions requires identifying and empowering local Digital Champions. These peer-led advocates bridge the gap, proving that digital tools—when designed for high-friction, low-resource settings—can be mastered through Modular, hands-on training rather than academic theory.
- Standards & Infrastructure: Adopting global standards and addressing the maintenance and continuity gap in government hospital hardware to support clinical reliability.
NRCeS: Facilitating National Adoption
The success of digital health depends on a single point of contact for standards and implementation support.
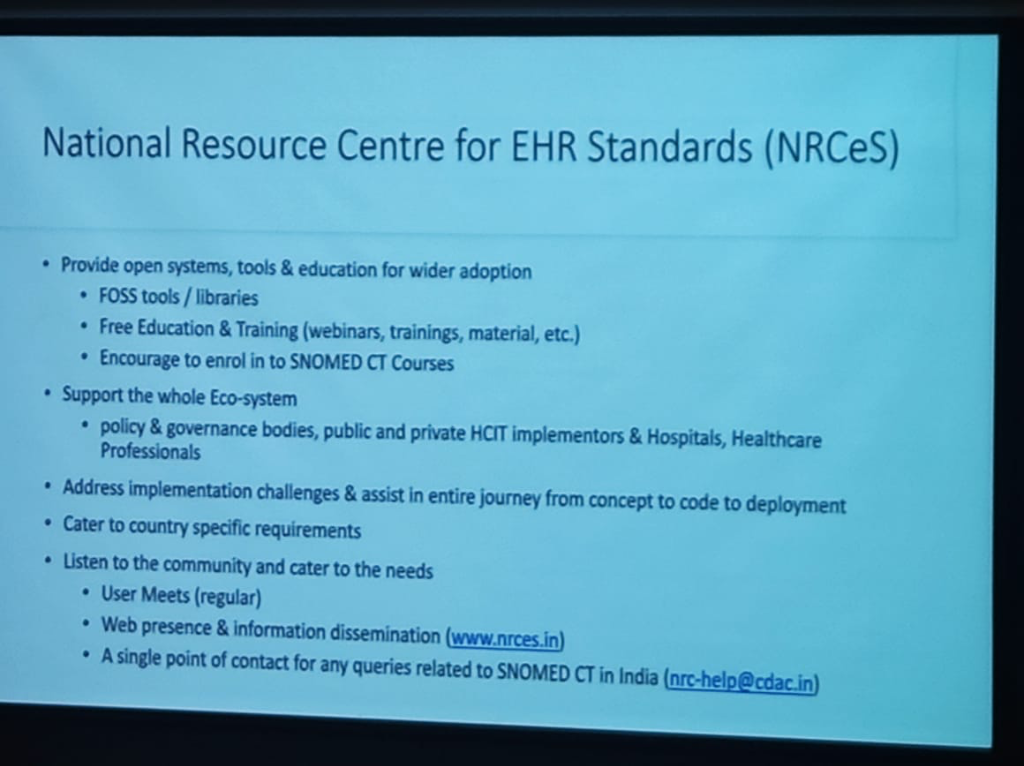
- Standards Development & Stewardship: NRCeS facilitates the adoption of notified EHR standards for India and acts as a knowledge base for associated resources.
- Co-Development & Implementation: They assist in the development of building blocks for national health missions (NDHM/ABDM) and provide hands-on implementation support to hospitals and clinicians.
- The "UPI of Healthcare": Just as UPI revolutionized finance, ABDM serves as the unified national backbone for health data exchange.
National Strategy: Entrepreneurship & ABDM (Dr. Thanga Prabhu)
A landmark moment at KCDH, IIT Bombay was the session led by Dr. Thanga Prabhu (MBBS, Emergency Medicine Specialist, former CMIO for Apollo Hospitals). With over a decade of experience in Emergency Medicine across Abu Dhabi and the UK, Dr. Prabhu brought a global clinician's perspective to the inauguration of the pan-India awareness campaign for the Ayushman Bharat Digital Mission (ABDM).
- The Bahubali Metaphor: Dr. Prabhu opened with the image of the GSLV Mark III, popularly known as "Bahubali"—India's heaviest rocket. This was not just a tribute to space exploration, but a metaphor for India's massive technical capability. ABDM is envisioned as a similar "moonshot" for healthcare.
- Make in India: Engineering Self-Reliance: A core message was the shift toward absolute self-reliance. India no longer needs to import digital health infrastructure. Just as the country built the Param Supercomputer when denied foreign technology, it is now building its own health-tech ecosystem. India is now the "Manufacturing and Engineering Capital" for the world.
- The Trust Deficit: A critical "trust deficit" currently faces the private healthcare ecosystem. When patients visit private facilities today, there is often uncertainty about whether a procedure is for the patient's benefit or the hospital's bottom line.
- The Rethink of Healthcare: ABDM represents a complete rethink of the ecosystem. Just as the government took responsibility for education and healthcare through institutions like IIT and AIIMS, it is now building the digital infrastructure to restore trust and transparency.
Ayushman Arogya Mandirs: The Primary Care Network
India is transforming its primary healthcare through a massive, 400,000-node network, operating under the supreme tagline: "Arogyam Paramam Dhanam" (Health is the Supreme Wealth).
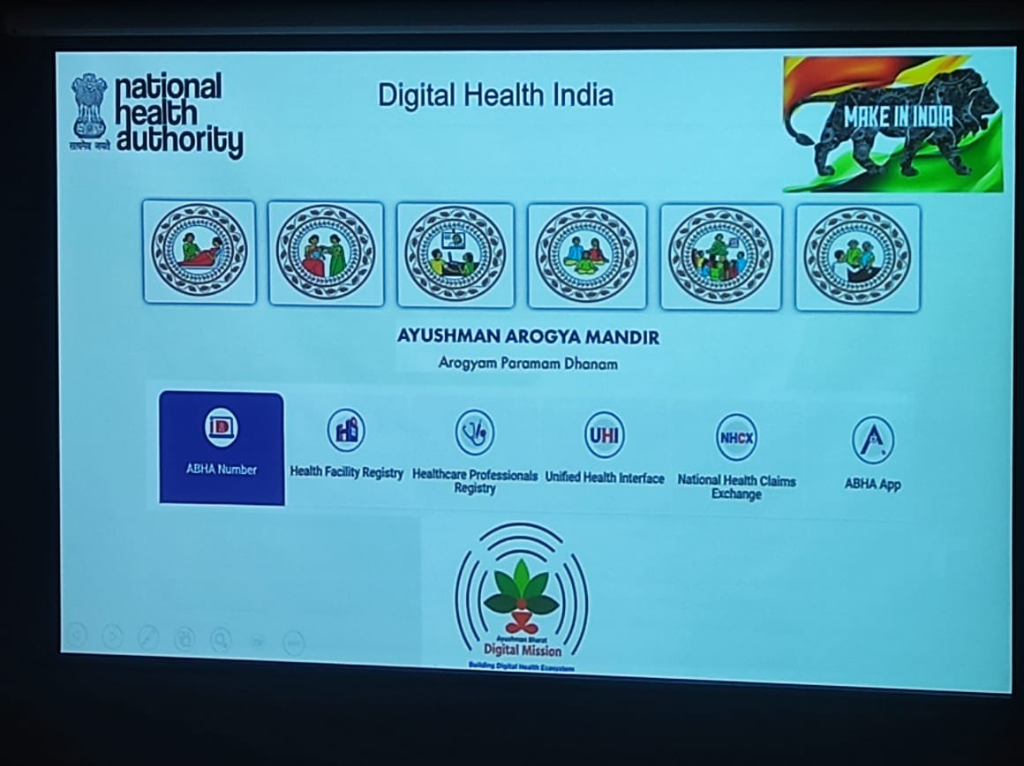 Figure: The National Health Authority's architectural vision for Digital Health India, showcasing the Ayushman Arogya Mandir pillars and the national digital backbone.
Figure: The National Health Authority's architectural vision for Digital Health India, showcasing the Ayushman Arogya Mandir pillars and the national digital backbone.
-
The Six Pillars of Frontline Care: The Arogya Mandir framework is visualized through six core service categories:
- Maternal Health: Comprehensive care for pregnancy and childbirth.
- Child Health: Neonatal, infant, and adolescent care.
- Tele-consultation: Bringing specialized care to remote areas via digital links.
- Reproductive Health: Family planning and reproductive services.
- Communicable Diseases: Management of common infectious diseases and outpatient care.
- NCD & Wellness: Screening and management of non-communicable diseases, alongside yoga and community wellness.
-
Transition from PHCs: What started as 25,000 Primary Health Centers (PHCs) at independence has evolved into 400,000+ Ayushman Arogya Mandirs (formerly Health and Wellness Centers).
- The Geriatric Priority: In a move that addresses a globally neglected segment, India's new primary care framework places a dedicated focus on Geriatric Medicine (60+ care). While the world often ignores the elderly, the Indian model integrates them into the frontline digital health loop.
The National Digital Backbone
Supporting these frontline "Mandirs" is a robust set of five digital pillars defined by the National Health Authority (NHA):
- ABHA Number: The unique digital identity for citizens.
- Health Facility Registry (HFR): The master database of verified healthcare facilities.
- Healthcare Professionals Registry (HPR): The directory of verified doctors, nurses, and paramedical staff.
- Unified Health Interface (UHI): The open protocol for digital health services (the "UPI of health").
- National Health Claims Exchange (NHCX): The gateway for seamless, paperless health insurance claims.
Ecosystem Triangulation: Identity, Verification, and Discovery
A critical architectural nuance shared during the session was the "Triangulation" model of the ABDM ecosystem. True trust is built by triangulating three verified sources of identity, complemented by secure storage and discovery layers:
- ABHA (Identity): Provides the persistent, across-the-board identity that anchors a citizen's longitudinal health story.
- HPR (Healthcare Professionals Registry): Ensures the provider is a verified health professional.
- HFR (Health Facility Registry): Ensures the care is delivered at a verified health facility.
- DigiLocker (Verification): Acts as the secure, government-verified repository for static "credentials" (e.g., insurance policies, vaccination certificates, and academic degrees).
- Discovery Layer (PHR/HIE): Enables the real-time "discovery" and fetch of dynamic clinical records (e.g., lab reports, discharge summaries, and prescriptions) from disparate hospital nodes.
NHCX: The 30-Second Claim
A major breakthrough in the ABDM architectural roadmap is the National Health Claims Exchange (NHCX).
- The Efficiency Goal: Currently, insurance claims are bogged down by manual verification and paper-heavy workflows. NHCX aims to transform this into a 30-second automated approval flow.
- The "UPI" for Claims: By triangulating Identity (ABHA) and Eligibility (Insurance credentials in DigiLocker), NHCX allows for near-instant validation of clinical necessity and coverage, drastically reducing the "Trust Deficit" between providers, patients, and payers.
ABDM: The Biggest Startup Opportunity
Dr. Prabhu issued a strong call to action for innovators, framing ABDM as the "Biggest Startup Opportunity" in the country today. Drawing on his experience as CMIO, he detailed a structured roadmap for where innovation is most needed.
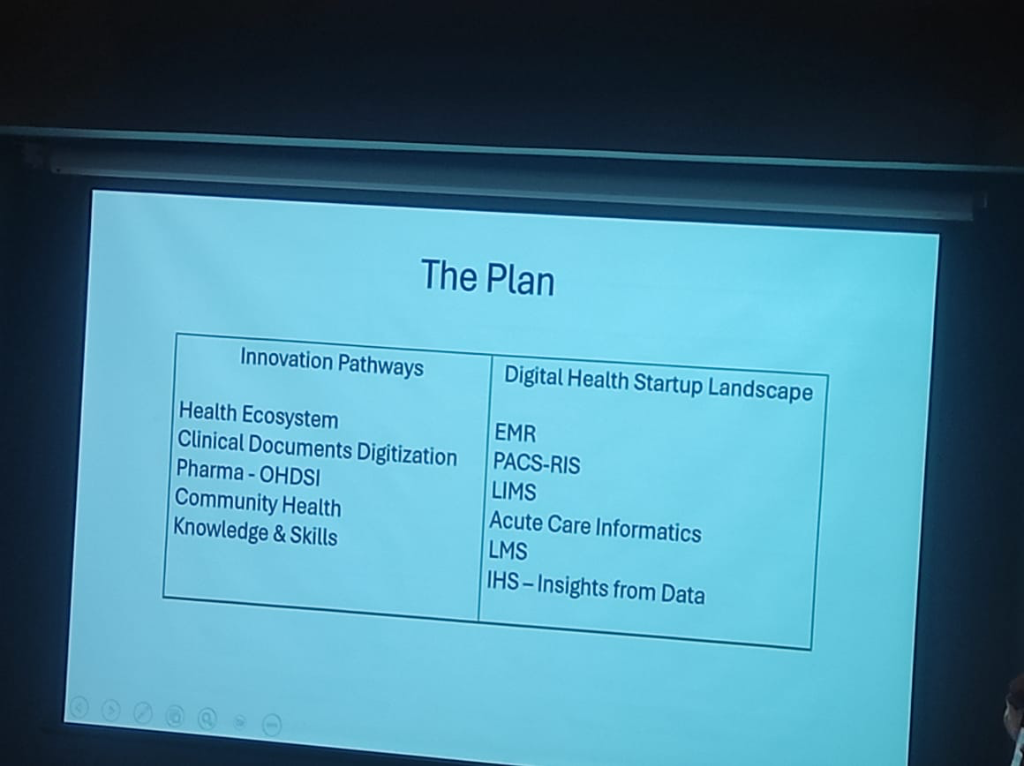 Figure: The strategic plan for digital health innovation pathways and the startup landscape.
Figure: The strategic plan for digital health innovation pathways and the startup landscape.
| Innovation Pathways | Digital Health Startup Landscape |
|---|---|
| Health Ecosystem | EMR (Electronic Medical Records) |
| Clinical Documents Digitization | PACS-RIS (Imaging & Radiology) |
| Pharma - OHDSI | LIMS (Laboratory Info Systems) |
| Community Health | Acute Care Informatics |
| Knowledge & Skills | LMS (Learning Management Systems) |
| IHS (Insights from Data) |
- Innovation at Scale: With 51 innovators already registered at the session's outset, the mission is designed for those who want to solve national problems while building sustainable businesses.
Federated Architecture: Resilience Through Decentralization
A core architectural tenet of the ABDM is the shift from a centralized to a Federated Architecture.
- Decentralized Nodes: Unlike legacy systems where a single point of failure can bring down the entire network, the national backbone is composed of independent, federated nodes.
- Isolating Failure: This design ensures that if a specific facility or region's node is affected—whether by technical downtime or a security incident—it does not hamper the others. The rest of the national ecosystem continues to function seamlessly, ensuring systemic resilience.
- Institutional Autonomy: Facilities maintain control over their data nodes, reinforcing the "Blind-to-Transit" model where the NHA provides the discovery layer without owning the clinical blocks.
The PHR Storage Paradox: Why 1GB Isn't Enough
A critical realization in the national rollout is the storage bottleneck facing Personal Health Record (PHR) applications.
- The DigiLocker Limit: While DigiLocker is a foundational pillar of India's digital infrastructure, it currently provides 1GB of storage. For a lifetime of clinical-grade data—including high-resolution diagnostic imaging and long-term inpatient summaries—this 1GB ceiling is not a viable repository for a comprehensive PHR.
- The "Google Pay" Model for Health: Consequently, the ecosystem is shifting toward a transactional model. Just as Google Pay does not "store" your money but provides a discovery and transaction layer for your bank accounts, modern PHR applications are evolving into Discovery & Transaction Gateways.
- Discovery First: In this model, the PHR app's primary role is to discover records across diverse providers (the "banks") and facilitate their secure, consent-based exchange, rather than serving as a monolithic cloud storage bucket for all clinical assets.
Anonymized Data: The Population Health Asset
While individual records are strictly governed by consent, the mission is unlocking clinical insights at scale through Anonymized Population Data.
- Aggregate Research: Frameworks are being operationalized to make anonymized, aggregated data available for public health research, disease surveillance, and national policy planning.
- Privacy-First Surveillance: By decoupling individual identity from clinical trends, the ecosystem can monitor healthcare efficacy and disease patterns in real-time, creating a national asset for medical research and AI training without compromising privacy.
International Portability: Sovereign Conversations
The vision for Indian digital health extends beyond national borders, aiming for seamless International Portability of health records.
- Ongoing Sovereign Discussions: While the technical baseline (HL7 FHIR) is global, formal cross-border data exchange remains a subject of active Soverign Government Discussions.
- Bilateral Protocols: Integration with international health systems is being negotiated at the diplomatic level to ensure that cross-border integrations are both secure and formally recognized by participating nations.
- Education & Training: NRCeS provides free training—including SNOMED CT courses—to support the whole ecosystem.
- Open Systems & Tools: By providing FOSS tools and libraries, NRCeS address implementation challenges through regular community engagement.
Success at Scale: IPD Linkage in Bihar
While many states are still focusing on OPD, Bihar has emerged as a leader in complex record linkage. - IPD Record Portability: Bihar has successfully operationalized the linking of In-patient (IPD) records to the ABHA ID. - Live Proof-of-Concept: This demonstrates that even narrative-heavy inpatient summaries can be structured and shared across the national backbone, providing a blueprint for other states to follow.
NHA Auditing & Governance: The Blind-to-Transit Reality
To combat the "shortcut" culture, the NHA and NHM teams are evolving their roles from facilitators to Auditors of Implementation Quality. However, this auditing is governed by a fundamental architectural constraint:
- Zero-Visibility (Blind-to-Transit): The NHA has no visibility into health data while it is in transit or at rest. They only provide the discovery and consent layer. This is a deliberate privacy-first design choice.
- Fiduciary Responsibility: Because the NHA cannot "see" the data, the Hospital (the fiduciary) remains solely responsible for any missing, inaccurate, or incomplete documentation. The responsibility for data presence and integrity stays at the clinical source.
- Quality Auditing: NHA's role is to ensure that the software implementers provide the capability for structured data, but the onus of population and accuracy remains with the originating institution.
Advanced Implementation Insights: Agency, Scale, and Friction
The evolution of India's digital health mission is uncovering deep technical and regulatory insights into how scale and agency are truly achieved.
Patient Agency: The PHR Link Model
A core tenet of the ABHA ecosystem is empowering the patient as the primary orchestrator of their medical history.
- The Push Mechanism: Instead of a central repository, the system uses a Link and Share model. Patients receive a digital link (via PHR apps like the ABHA app) to their clinical records for both Out-patient (OPD) and In-patient (IPD) care.
- Longitudinal History: By linking these fragmented visits, the patient maintains a continuous, longitudinal health record that they can share with any clinical provider, regardless of the hospital's internal HIS.
Population Health & The ABHA Aggregate
Beyond individual care, the digitization of clinical records opens the door to massive Population-wide Health Insights.
- Aggregated Data for Trends: The federated architecture allows for the collection of anonymized, aggregated data to track disease outbreaks, treatment efficacy, and public health trends at a national level.
- Research Partnerships: This data serves as a critical asset for academic and clinical research, enabling partnerships between the NHA, research institutions, and the private sector to drive evidence-based medicine.
Data Without Borders: International Portability
The technical standards adopted by India (FHIR, SNOMED CT) are designed with International Interoperability in mind.
- Cross-Border Continuity: The next frontier is enabling the portability of health records for Indian citizens traveling or living abroad, ensuring that their medical history is accessible and semantically understood by global healthcare systems.
- Global Standards Alignment: By adhering to international norms, India ensures that its digital health infrastructure is compatible with emerging global health data exchange frameworks.
The Private Sector Paradox: Regulatory & Operational Friction
While the government sector has shown aggressive adoption, the private sector faces unique Implementation Frictions.
- Licensing & Compliance (DMHO): Private hospitals often navigate a complex regulatory landscape, where digital adoption is linked to DMHO Licensing and other state-level compliance "sticks."
- The Mandate Gap: Unlike government-led institutions, private hospitals must balance the high cost of digital transformation with operational profitability, often leading to a slower adoption curve unless mandated by national insurance schemes or regulatory requirements.
- Strategic Concentrate: As a result, the most robust "advanced" implementations are currently concentrated in large public sector institutions, creating a "digital maturity gap" that the next phase of the mission aims to close.