Part V: Human-Centric Implementation
Doctors & Nurses: At the Frontlines of Change
Crucially, the transformation of healthcare cannot be a purely technical endeavor. Clinicians must lead innovation.
- Brilliant Ideas: Clinicians on the front lines have the most profound insights into system gaps.
- Adaptation Pressure: There is immense pressure on clinicians to adapt to digital systems. Resistance often stems from the "key-in vs. writing" friction; tools must reduce, not increase, the operational load.
- Strategic HIS Success: HIS succeeds when a core group of doctors and nurses lead the effort from the ground up, tailoring the system to specific hospital needs before heavy capital investment. Since no two hospitals function the same way—each having its own unique clinical SOPs—clinicians must lead this customization.
- Workflow Variability: As emphasized by Prof Supten Sarbadhikari, clinical workflows (including ADT—Admission, Discharge, Transfer) are not standardized globally. They vary by hospital, department, and even individual doctor, making software adaptability a critical success factor.
- The Problem of Legacy Migration: Migrating from legacy systems is a major hurdle. While starting from scratch is technically simpler, established institutions face the immense friction of data migration and system continuity.
- User Resistance Spectrum: Resistance isn't binary. KCDH identifies a spectrum of users: from those who are highly motivated but difficult to train, to those who are easy to train but difficult to motivate. A major cultural hurdle is the mismatch between motivation and training; in many institutional settings, the leader is the least motivated for digital change, creating a top-down stagnation.
- The Horse to Water Analogy: Implementation and deployment are the "easy parts"—if administration mandates it, it will happen. However, making people use the system is the real challenge. True adoption requires deep cultural change management.
- Learning, Unlearning, & Relearning: Success requires a continuous human cycle of learning, unlearning, and relearning as clinicians transition through technological generations.
- Technology Lifecycle: Digital health is not a one-time investment. Just as mobile technology advances in 1-2 year cycles, health systems must be built for continuous upgrades to remain clinically relevant and secure.
- Data Quality & Integrity: A foundational but often overlooked requirement. Standards like SNOMED CT provide the structure, but the cleaning, structuring, and integrity of data entered are paramount for operational continuity.
- The Cost of Redundancy: Redundant data entry is more than just a nuisance; it is expensive, frustrating, and a waste of time that detracts from patient care.
- Trust as a Foundation: For digital transformation to succeed, there must be a fundamental foundation of Trust. Patients and clinicians must trust that "my hospital data" is handled with the utmost integrity.
The Capacity Building Framework
To overcome the "Fixed Mindset" barrier, KCDH emphasizes a holistic approach to Capacity Building that fosters Cultural Agility:
- Consent-Driven Architectures: Aligning with the ABDM framework, data sharing must be built on Consent-Driven Architectures that ensure Ethical Data Sharing and patient agency.
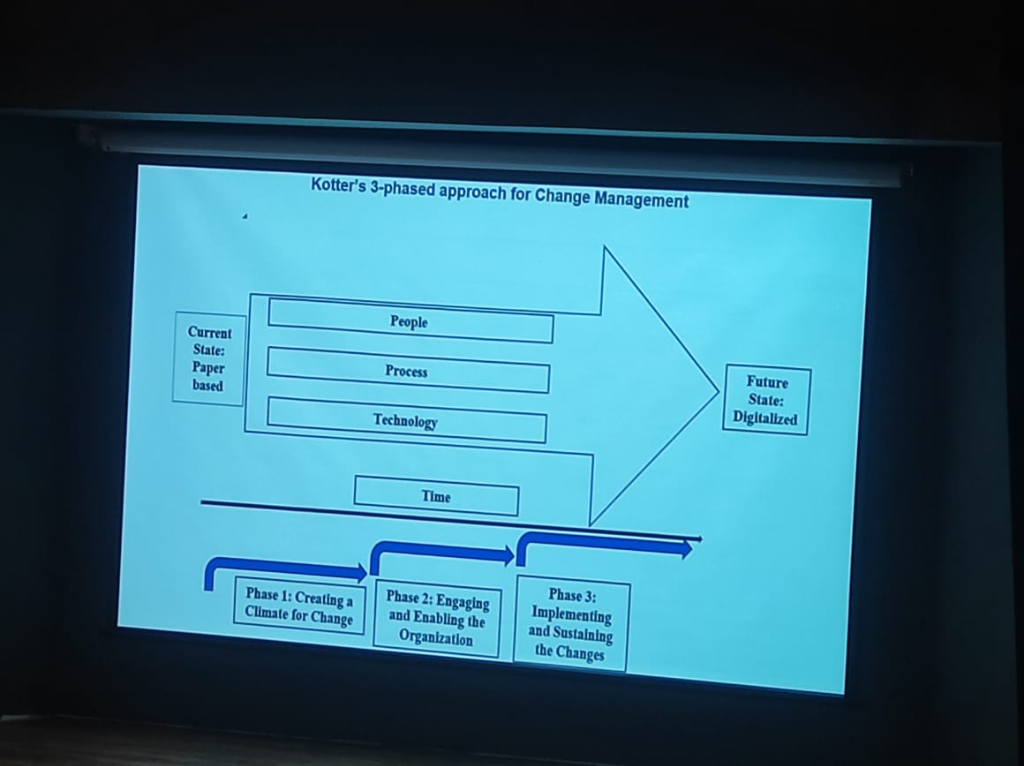
- Change Management (Kotter's 3-Phased Approach): Real transformation follows a structured journey of creating a climate for change, engaging the organization (through Champions), and finally sustaining the gains.
- Tailored Modules: Customizing digital tools for doctors and paramedical staff to ensure they serve clinical reality rather than a generic vendor vision.
- Clinician control: Physicians can audit all automated processes, ensuring that AI remains a "Decision Support" tool rather than a replacement for clinical judgment.
Clinical Safety: Safer Medications, Better Care
As highlighted by Sonali Deshmukh (MIMS Clinical Decision Solutions), the digitalization of the hospital is a prime opportunity to enhance medication safety.
- Clinical Decision Support (CDS): Moving from simple e-prescribing to intelligent systems that provide real-time alerts for drug-drug interactions, drug-allergy contraindications, and dosage errors.
- Evidence-Based Prescribing: Integrating medical knowledge bases (like MIMS) directly into the clinician's workflow to ensure that prescribing is grounded in the latest clinical evidence.
- Closing the Loop: Technology allows for "closing the loop" on medication administration—ensuring the right drug reaches the right patient at the right time through barcoding and automated pharmacy systems.
Institutional Standards: NABH & The Maturity Path
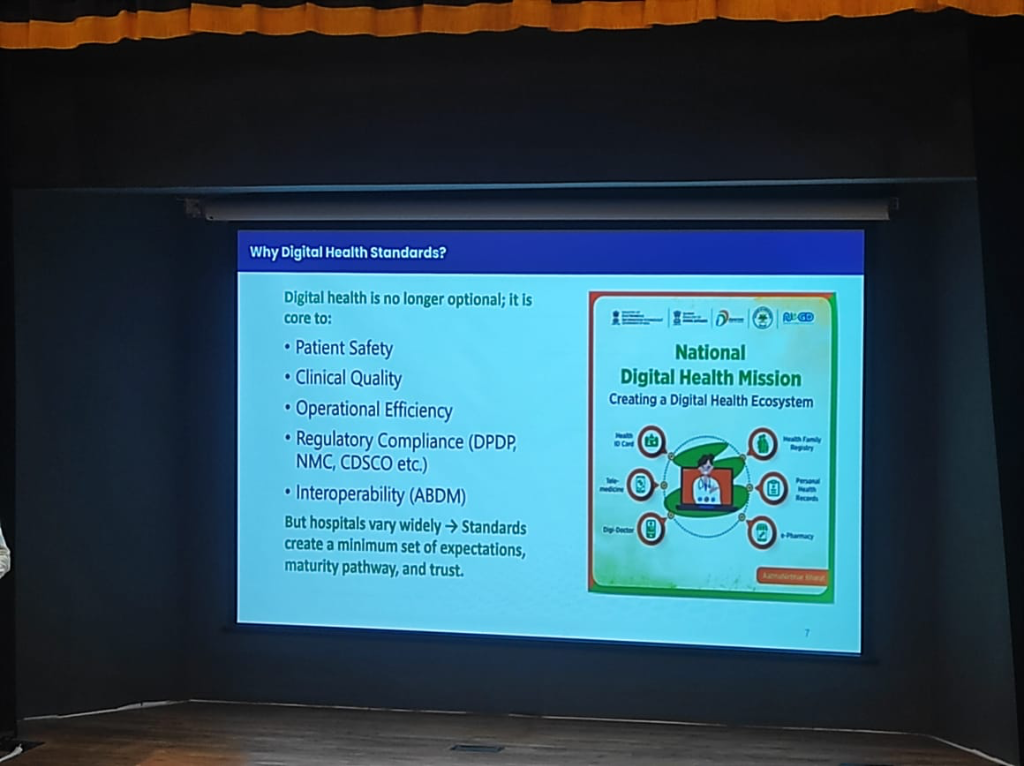 Figure: The National Digital Health Mission ecosystem, creating a unified pathway for patient safety and interoperability.
Figure: The National Digital Health Mission ecosystem, creating a unified pathway for patient safety and interoperability.
JCI vs. NABH: A Global-Local Bridge
A common question arises regarding the choice between international and national standards. While JCI (Joint Commission International) is a prestigious global benchmark, it is primarily designed for western, developed contexts where patient quality awareness and secondary infrastructure are already at a high baseline.
- The India Reality: India requires a Tiered Approach. NABH standards are explicitly designed to account for varying institutional strength, digital maturity, and geographic location (Tier 1 vs. Tier 2/3).
- Progressive Maturity: Instead of a "pass-fail" global hurdle, NABH allows hospitals to grow through tiered accreditation, making quality excellence achievable for everyone from a rural 30-bed hospital to a metropolitan multi-specialty center.
The 8-Chapter Modular Framework
To ensure structured and progressive growth, the NABH digital standards are organized into eight key chapters, covering both clinical and operational excellence:
- AAC (Access, Assessment, and Continuity of Care): Streamlining Admission, Discharge, and Transfer (ADT) and ensuring long-term care continuity.
- COP (Care of Patients): The clinical heart of the framework, digitizing core care pathways and real-time patient monitoring.
- MOM (Management of Medication): Standardizing the entire medication lifecycle, from pharmacy inventory to safe bedside administration.
- HRM (Human Resource Management): Managing the clinical and administrative workforce in a structured, digitized environment.
- IMS (Information Management Systems): Breaking down data silos to ensure True Portability of health records across the institution.
- Finance & Procurement (P&L): Transparent tracking of clinical consumables and financial throughput.
- Digital Infrastructure & Security: Foundational standards for hardware maintenance and data protection.
Breaking the Silos: A Unified Mission
As Avinash Pandey highlights, one of the greatest contributions of NABH digital standards is their ability to break organizational silos.
- The Trinity of Adoption: Successful EMR adoption is no longer just an "IT project." It is a unified mission where the Clinical, Quality, and IT teams come together.
- Standardized Quality: Quality teams provide the data integrity benchmarks, clinical teams provide the operational reality, and IT teams provide the technical backbone. This cross-functional collaboration is the key to moving from fragmented data to a cohesive digital health ecosystem.
Small-Hospital Scalability: Design for India's Reality
A common misconception is that digital standards are only for large corporate hospitals. On the contrary, NABH standards are explicitly designed to be inclusive of 30-50 bed hospitals, which form the backbone of Indian healthcare.
- Remote Adoption: Small hospitals in remote regions—from Manipur to Jammu & Kashmir—are already adopting these standards, proving that digital maturity is a function of leadership more than bed count.
Lightweight EMR Strategies: Pragmatic Digital Adoption
One of the most significant insights from the current national rollout is that Small and Medium healthcare facilities need not have a full-fledged, complex EMR to participate in the digital ecosystem.
- Micro-EMR Solutions: The NHA is actively collaborating with and promoting lightweight platforms like eSushrut and eKa Care. These solutions provide the core digital building blocks (ABHA linkage, consultation logging, and report sharing) without the overhead and cost of a Tier-1 enterprise system.
- Modular Growth: This strategy allows smaller clinics and nursing homes to achieve basic digital compliance almost immediately, with the path to add more complex clinical modules as they scale or their needs evolve.
- Democratizing Quality: By lowering the entry barrier, even a small community hospital can achieve the same data integrity and patient safety benchmarks as a Tier-1 institution.
The ROI of Standards: Measurable Impact
Standards are not just about compliance; they are a direct driver of institutional revenue and operational velocity. Reported improvements from hospitals adopting national digital health standards include:
- Revenue Velocity & Throughput:
- 30% Average Reduction in Patient Waiting Time: Dramatically increasing patient volume and clinic efficiency.
- 20% Reduction in Discharge TAT: Faster bed turnover, allowing for more revenue-generating admissions in the same fixed facility.
- Revenue Capture & Operational Savings:
- 18% Reduction in Prescription Bounces: Direct revenue growth for hospital pharmacies by ensuring internally generated prescriptions are captured at the point of care.
- 39% Diagnostic & 15% Blood Component TAT Reduction: Faster clinical decision-making, reducing uncompensated "stagnation" time.
- Risk & Clinical Excellence:
- 10% Medication Accuracy Improvement: A critical shield against clinical errors, litigation, and adverse patient incidents.
- 100% Patient Record Access: Realizing the longitudinal health record, reducing redundant testing and improving diagnostic precision.
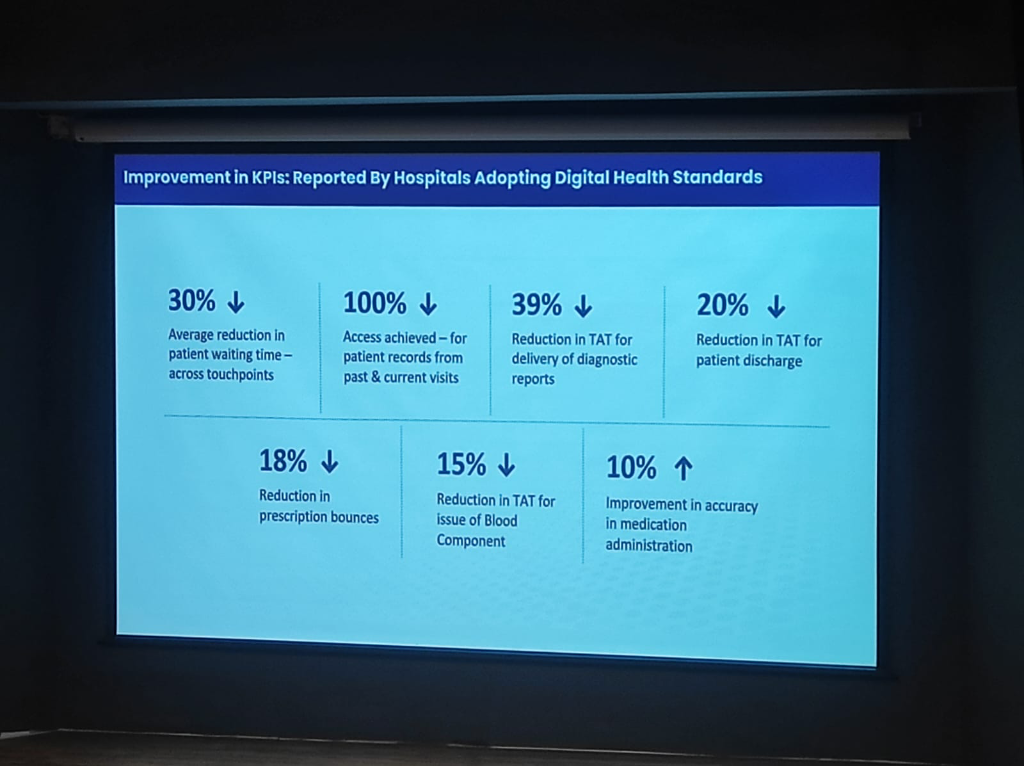 Figure: Measurable KPI improvements reported by hospitals adopting national digital health standards.
Figure: Measurable KPI improvements reported by hospitals adopting national digital health standards.
The Certification Shortcut vs. The Impact Gap
For hospitals looking to accelerate their accreditation, NABH has simplified the compliance burden. Institutions that adopt NABH-certified HIS, EMR, or Practice Management Systems (PMS) are automatically considered compliant with the digital standards. This ensures that even smaller clinics can achieve standardized quality without needing a massive internal IT department.
However, a critical distinction exists between Certification and Operational Impact:
- The M1/M2/M3 Gap: While many systems are certified for Milestones (M1/M2/M3), the actual implementation often falls into the "Photo-Upload" Trap. Instead of capturing structured, clinical-grade data, some implementers simply upload photos of paper records to meet compliance.
- Structured Data for AI: This shortcut renders the data useless for AI-driven clinical decision support. True impact requires native structured data entry at the point of care, moving beyond simple digitization of paper.
Financial & Resource Support: Bridging the Digital Divide
Achieving digital maturity represents a significant capital and operational investment, especially for smaller institutions.
- The Funding Hurdle: Small hospitals (30-50 beds) require dedicated support for Hardware Procurement, reliable connectivity, and specialized Manpower for data entry and system maintenance.
- Government Assistance: There is an urgent need for financial subsidies or grant frameworks from the government/NHA to offset these initial costs, ensuring that digital health doesn't become a "Tier-1 only" privilege.
Health Data Retention & Private Sector Friction
The path to universal adoption is paved with both policy mandates and legal complexities.
- Health Data Retention Policy: The NHA has launched a comprehensive Health Data Retention Policy. Any HMIS or health facility integrating with the national backbone must adhere to these standardized retention timelines, ensuring that longitudinal records are not prematurely archived.
- The Lobby Constraint: Despite the government's push, private sector participation remains significantly lower. In some states, attempts to mandate ABDM were met with strong opposition from medical lobbies, resulting in court stay orders that have temporarily halted aggressive implementation. The strategy has thus shifted from "force" to "facilitation and awareness."
Design Thinking: Innovation for India
Dr. Richa Singh outlined a foundational framework for healthcare product development in the Indian context, centered on First Principles.
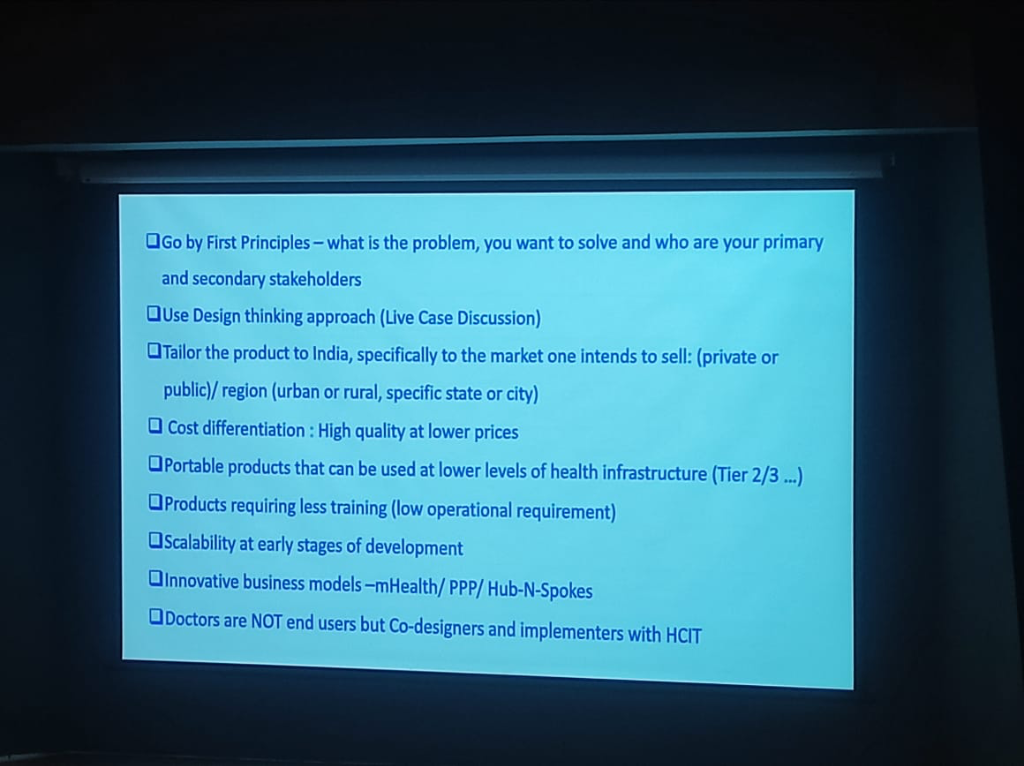 Figure: The design thinking framework for tailoring healthcare products to the Indian market.
Figure: The design thinking framework for tailoring healthcare products to the Indian market.
- Go by First Principles: Success starts with identifying exactly what problem you want to solve and who the primary and secondary stakeholders (clinicians, patients, administrators) are.
- Tailor to the Market: Products must be specifically adapted for the segment they intend to serve:
- Sector Specific: Different strategies for Public vs. Private sectors.
- Region Specific: Accounting for Urban vs. Rural needs, or specific city/state dynamics.
- The India Vectors: Direct integration of native Languages and the ABHA/ABDM identity stack is no longer optional.
- Cost Differentiation: Achieving high quality at significantly lower prices is the benchmark for Indian innovation.
- Doctors are NOT End-Users: A critical paradigm shift is treating doctors as Co-designers and implementers rather than just passive users.
- Workflow is King: Clinicians will not change their existing workflow to suit an app or developer. The technology must instead bend to the clinical reality.
- The Burden of Choice: If a tool requires a doctor to carry an extra device (e.g., a specific digital pen) or adds friction to an emergency, it will be rejected.
- Portability & Scalability:
- Low Level Infrastructure: Designing portable products that function reliably in Tier 2/3 cities.
- Low Operational Requirement: Minimizing the training burden on the healthcare workforce.
- Early-Stage Scalability: Ensuring the product architecture can scale from Day 1.
Phygital Delivery: Bridging the Last Mile
Another core theme presented by Dr. Richa Singh is the Phygital (Physical + Digital) model, which acknowledges that technology alone is insufficient in the Indian context without a robust physical touchpoint layer.
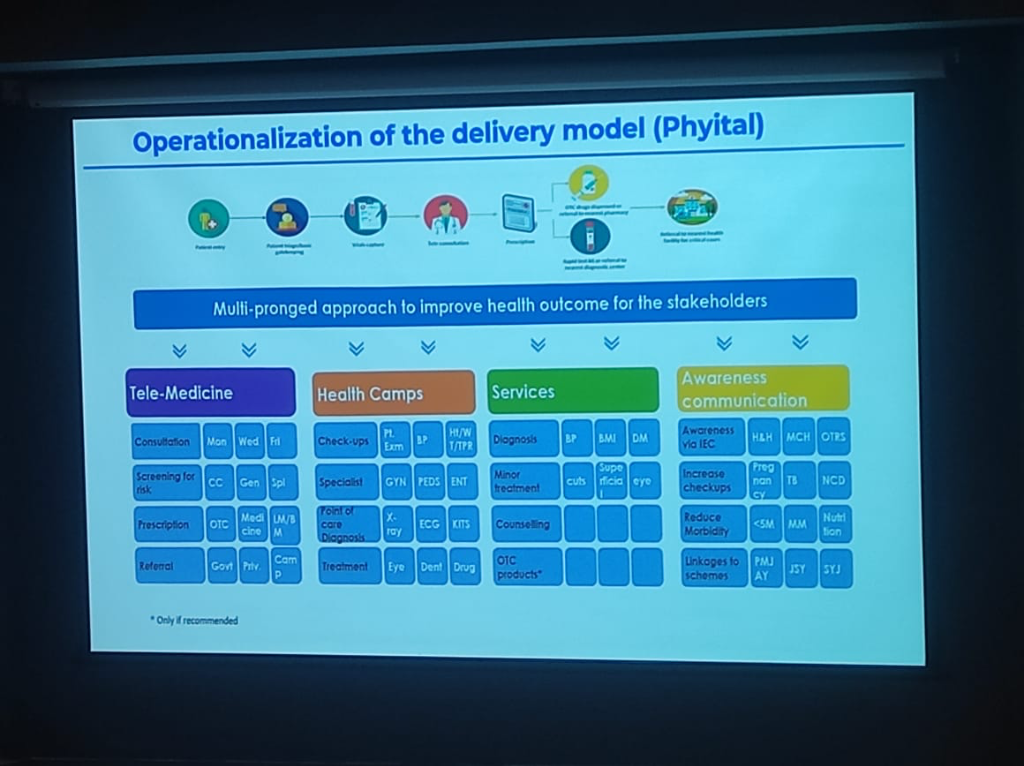 Figure: Operationalization of the Phygital delivery model, integrating community health gates with digital consultations.
Figure: Operationalization of the Phygital delivery model, integrating community health gates with digital consultations.
- The Phygital Patient Journey:
- Community Gatekeeping: The journey begins with Anganwadi and ASHA workers who act as the primary physical triage layer.
- Vitals & Triage: Patient information and vitals are captured at the community level before escalation.
- Digital Bridge: Tele-medicine connects these community hubs to specialists, ensuring that distance is no longer a barrier to quality care.
- Point-of-Care Diagnosis: Rapid test kits and referrals to nearest diagnostic centers complete the loop.
- Service Pillars:
- Tele-Medicine: Continuous consultation and risk screening.
- Health Camps: Periodic physical check-ups and specialist screenings.
- Diagnostic Services: Basic lab work and minor treatments delivered locally.
- Awareness Communication: IEC (Information, Education, and Communication) campaigns focused on Maternal and Child Health (MCH), Nutrition, and non-communicable diseases (NCDs).
Innovative Operational Models
To succeed in this environment, innovation must move beyond product-level technology to encompass service delivery and operating models.
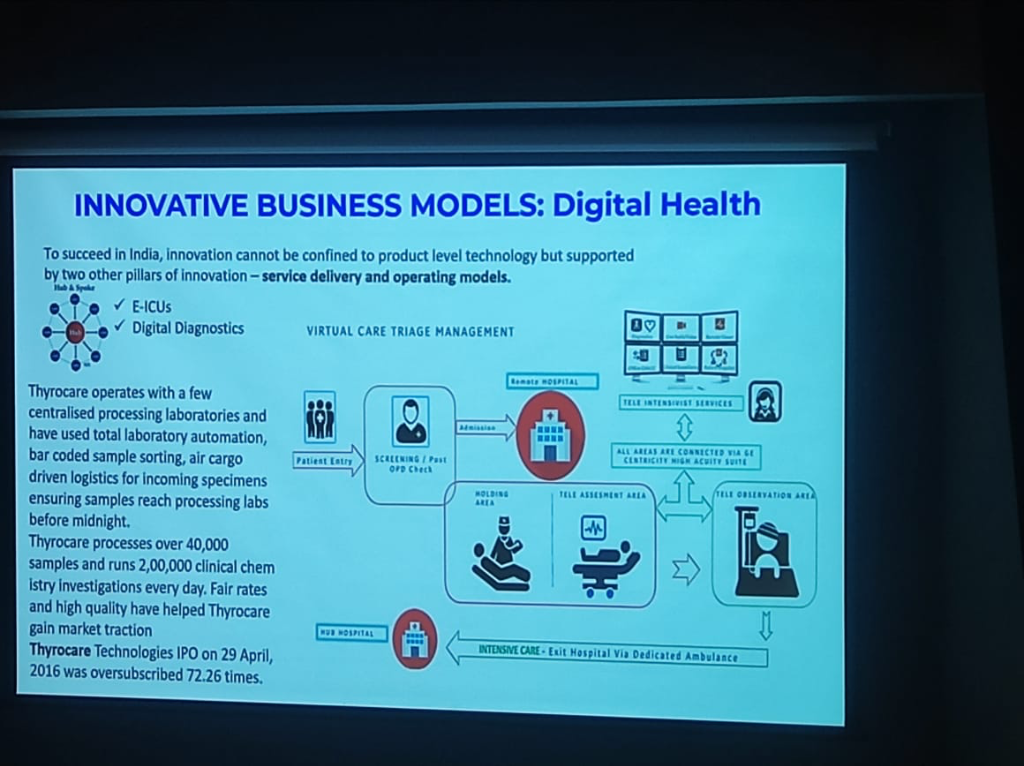 Figure: Innovative business and operating models in the digital health ecosystem.
Figure: Innovative business and operating models in the digital health ecosystem.
- Centralized Hub-Spoke Lab Model (e.g., Thyrocare):
- Hub-Spoke Architecture: A massive decentralized network of collection points (spokes) feeding into centralized processing hubs.
- Overnight Processing: Utilizing air cargo-driven logistics to ensure specimens reach one of the 4 centralized processing hubs by midnight.
- Total Automation: Implementing bar-coded sample sorting and end-to-end automated clinical chemistry paths.
- Scale & Efficiency: Processing over 200,000 investigations daily, proving that high-quality diagnostics can be delivered at fair rates through massive scale.
- Virtual Care Triage (e.g., GE Centricity):
- Remote Triage: Implementing Tele-ICU hub-and-spoke models where local teams are supported by remote specialists via high-acuity suites.
- MIoT Integration: Utilizing the Medical Internet of Things for continuous oversight of vitals and imaging across regional networks.
The Evolution of Clinical Data Entry
A transformative theme of the session was the shift away from traditional, cumbersome data entry toward intelligent, machine-driven workflows.
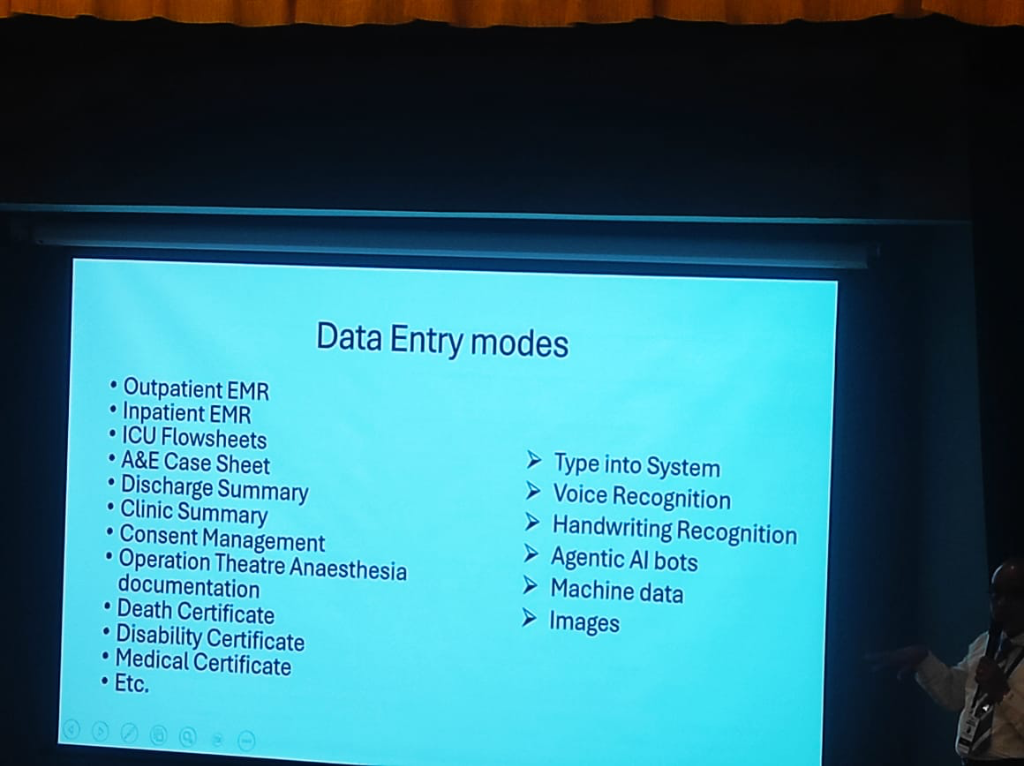 Figure: The transition from manual typing to Agentic AI and machine data in clinical environments.
Figure: The transition from manual typing to Agentic AI and machine data in clinical environments.
- The Document Spectrum: Dr. Prabhu highlighted the diverse array of complex clinical documents that require digitization to build a true longitudinal history:
- Acute Care: A&E Case Sheets, ICU Flowsheets, and OT Anaesthesia documentation.
- Certifications: Death, Disability, and Medical Certificates.
- Routine Care: Outpatient/Inpatient EMRs, Discharge and Clinic Summaries, and Consent Management.
- The Entry Modes: The roadmap moves beyond the "Type into System" era, embracing:
- Vendor Case Examples:
- Voice (Augnito): Grounding the vision of voice-first clinical workflows by referencing Augnito's high-accuracy, real-time medical dictation.
- Handwriting (DocsPro Pen / Doxper): Utilizing digital pens (like Doxper) as the bridge between paper-based workflows and digital data. However, this mode faces real-world adoption hurdles: doctors are reluctant to carry a second pen and fear the fragility of the device in high-pressure clinical moments.
- Rounds Notes (DailyRounds): Positioning DailyRounds as a specialized enterprise app for doctor rounds notes. In the "post-eSushrut" (C-DAC HMIS) era, such apps serve as a critical second layer, capturing deep clinical nuances and providing a superior user experience for bedside documentation that broad-based systems may miss.
- Machine Data & Images: Direct ingestion from medical devices and diagnostic imaging.
- Agentic AI Bots: As presented by Ms. Manini Puranik (Ekaaya), Agentic AI represents the primary future mode for data entry. This involves a fundamental shift from "typing into a system" to having autonomous agents that assist in capturing, structuring, and verifying clinical data in real-time.
Corporate Healthcare Dynamics
The private sector in India is evolving from traditional "hospitals" toward a model of "Hospitality in Hospitals", focusing on premium patient experience and standardized services.
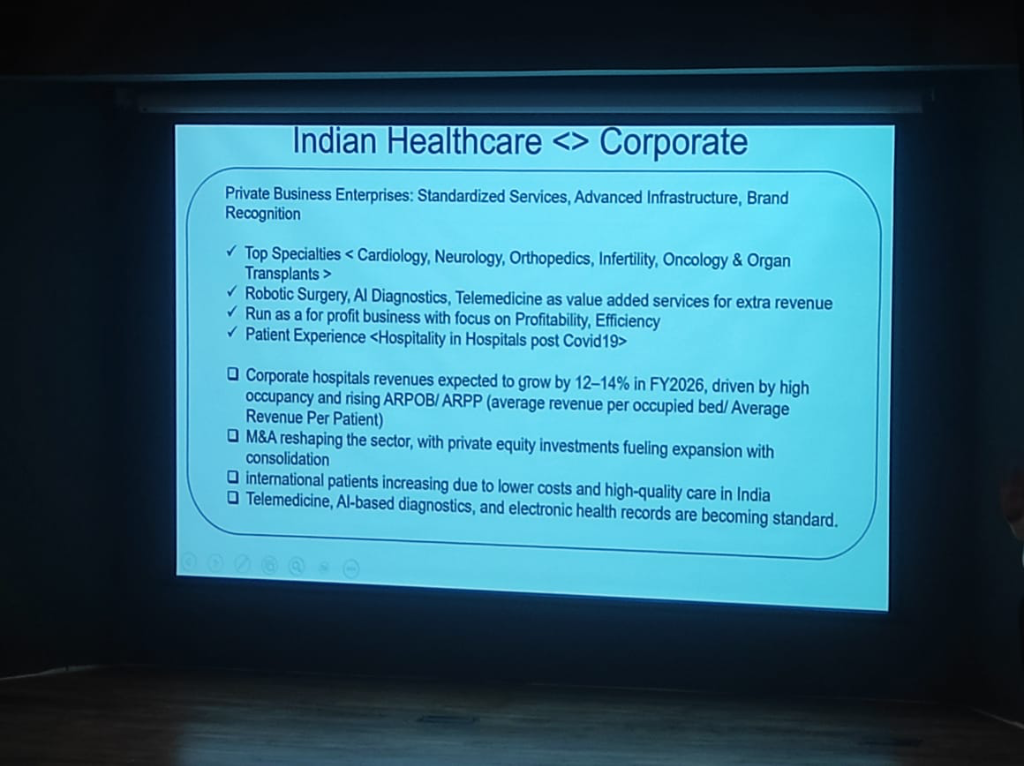 Figure: The operational and financial roadmap for India's corporate healthcare sector.
Figure: The operational and financial roadmap for India's corporate healthcare sector.
- Growth & M&A: The sector is seeing aggressive expansion and consolidation, with revenues expected to grow by 12-14% in FY2026, driven by high occupancy and rising ARPOB/ARPP (Average Revenue Per Occupied Bed/Patient).
- The Telemedicine Behavior Shift: Post-COVID, there has been a fundamental behavioral shift. The "remote culture" has moved Telemedicine from a backup option to a standard "value-added service." It is now an integral part of the patient experience and a key revenue engine.
- Revenue Engines: The sector is pivoting toward high-specialty services (Cardiology, Neurology, Oncology) and adopting high-tech drivers like Robotic Surgery and AI Diagnostics to maintain profitability and efficiency.
- Electronic Health Records: Integration with ABDM is becoming a standard requirement for private business enterprises to maintain brand recognition and operational parity.
The DNA of Excellence: An Indian Identity
Dr. Prabhu highlighted that the success of the digital mission is rooted in a unique "DNA of Excellence" driven by decades of national investment.
- From Shyness to Pride: While Indians are often "shy by nature" in claiming credit, Dr. Prabhu noted that the world's best companies are now run by Indians. This is the fruit of 30-40 years of deep investment in Education, Medicine, and Engineering.
- The Education Priority: Unlike many Western contexts, India places an unparalleled priority on education. The mantra of "study well and do well" is embedded in the cultural fabric, providing a high-quality human capital baseline for digital transformation.
- Global Leadership: This investment is now yielding fruit across all fields—Pure Science, Engineering, and Medicine—positioning India not just as a consumer of digital health, but as a global leader in its innovation and deployment.
Preventive-First: A Strategic Shift
A core theme of the session was the fundamental shift from curative-only to Preventive-First healthcare.
- The Cure Paradox: While curative medicine—transplants, cardiac procedures, and high-capital neurosurgeries—is necessary, its impact is limited by resources and cost.
- Community-First Care: Dr. Prabhu emphasized that health begins in the community. The strategic goal is to manage health before a person becomes a patient. If managed well in the community, they don't even need to enter the hospital, reducing friction and cost across the entire system.
- Population Health: The real benefit for India's population lies in Primary and Preventive Health. By focusing on lifestyle diseases and early intervention, ABDM aims to keep people out of hospitals rather than just managing them once they are there.
- Standardized Prevention: The digital mission provides the platform to operationalize this preventive strategy at a national scale, making it the "first point" of the whole ecosystem.
Home Healthcare: The Next Frontier
A significant shift highlighted by Dr. Prabhu is the transition from hospital-centric to Home-Centric Care.
- Delivering Care at Home: Technology now enables the management of long-term conditions (Diabetes, Hypertension) and post-acute recovery in the patient's home.
- Palliative & Mental Health: Palliative and end-of-life care, traditionally restricted to hospitals or nursing homes, can now be managed more humanely at home. Similarly, Mental Health services are being successfully delivered remotely.
- The Elderly Opportunity: Dr. Prabhu identified Elderly Care as the "next big opportunity" for the next 50 years—a sector that is currently neglected but holds massive potential for digital innovation.
- Connected Ambulances: By utilizing MIoT (Medical Internet of Things), ambulances are being transformed into "field clinical delivery" units, allowing for life-saving interventions before the patient even reaches the hospital.
Just-in-Time Skills: Rapid Upskilling
The rapid pace of digital transformation requires a fundamental shift in how we approach medical and technical education.
- Beyond the Classroom: The days of spending years in a college to learn a static skill set are over. The fast-moving digital health landscape demands Just-in-Time Skills.
- Real-Time Learning: Professionals must now be able to quickly ramp up on new technologies and protocols as they emerge. This shift toward continuous, real-time upskilling is critical for building the cadre needed to support the digital mission.
On-Premise vs. Cloud-Native: The Strategic Choice
Institutions must decide where their "brain" resides, balancing control with scalability.
| Feature | On-Premise (Legacy Control) | Cloud-Native (Modern SaaS) | Hybrid (The Indian Reality) |
|---|---|---|---|
| Hosting | Local server rooms with strict HVAC/Fire safety. | Hosted on secure data centers (AWS, Azure, Google). | Tiered: Critical Core on-prem; Scale/Analytics on Cloud. |
| Maintenance | Significant—requires on-site hardware engineers. | Lower—handled by the cloud provider. | Balanced: Internal IT + Managed Cloud Services. |
| Scalability | CapEx-intensive; requires buying new hardware. | Elastic; scales up/down based on demand. | Incremental: Buffer local, burst to Cloud for scale. |
| Connectivity | Fast local LAN; works during internet outages. | Dependent on high-availability internet. | Resilient: Core works offline; Syncs when online. |
| Initial Cost | High upfront investment (Hardware + Setup). | Lower entry cost (Pay-as-you-go). | Moderate: Selective hardware + Subscription OpEx. |
HMIS Governance: Indian vs. Overseas Providers
Choosing the right "brain" for the hospital depends on balancing global maturity with local clinical flexibility.
- The Intent Factor: Institutions with limited internal technical staff should prioritize Cloud-Native Indian providers that offer managed compliance.
- Geographic Reality: For hospitals in regions with internet instability, the Hybrid Deployment remains the gold standard to ensure clinical continuity during outages.
- Regulatory Resilience: Ensure your provider is ABDM-certified and provides a roadmap for DPDP Breach Liability management—this is no longer an optional feature.