Part VI: Public Health & Strategic Future
National TB Elimination Program: Breaking Taboos with AI
A powerful application of AI discussed by Dr. Richa Singh is its role in the National Tuberculosis Elimination Program (NTEP), where technology is being used to address both clinical and social challenges.
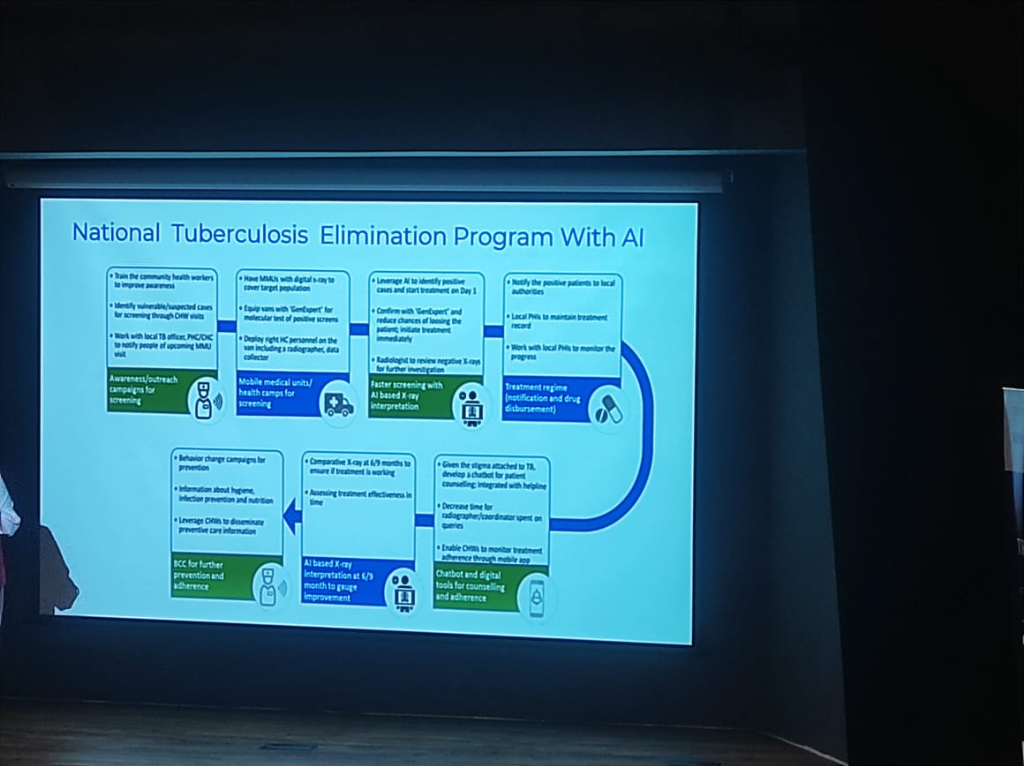 Figure: The AI-driven workflow for national TB elimination, from mobile screening to Day 1 treatment.
Figure: The AI-driven workflow for national TB elimination, from mobile screening to Day 1 treatment.
- AI-Driven Workflow:
- Mobile Medical Units (MMUs): Vans equipped with digital X-rays and AI-based X-ray interpretation software for faster screening.
- Day 1 Treatment: AI identified positive cases are confirmed via GenExpert molecular tests, aiming for treatment initiation on the very first day.
- Continuous Oversight: AI is used to review negative X-rays for further investigation and to gauge improvement via comparative X-rays at 6/9 months.
- Breaking the Stigma: The Trilingual Chatbot:
- The Taboo Challenge: TB carries a significant social stigma in many communities, often leading to delayed treatment.
- The AI Solution: A trilingual chatbot (supporting 3 languages) was developed for patient counseling and adherence.
- Outcome: Patients were found to be significantly less hesitant to interact with a bot than with a human for TB queries, bypassing the taboo and ensuring better engagement.
- Support Tools: The workflow incorporates Differential Diagnosis for lung conditions, Doc Scanners for digital records, and BCC (Behavior Change Communication) campaigns to improve awareness.
Digital Health Models: From Horizontal Scale to Clinical Trust
The Indian ecosystem is witnessing a diverse range of digital health applications, from broad platforms to trust-driven specialized models.
- Horizontal Scale & Profitability (e.g., Practo):
- Market Success: Practo is a primary example of a horizontal health platform that has achieved significant scale, gone public, and reached profitability.
- Core Offering: Focused on doctor discovery, appointment booking, and digital prescription infrastructure across a wide range of specialties.
- Crowdsourced Clinical Trust (e.g., Lybrate):
- Crowdsourced Intelligence: Lybrate specializes in providing second opinions through a crowdsourced model.
- Peer-Reviewed Trust: Its unique value proposition lies in the peer review of medical opinions, building a "trust layer" that navigates clinical uncertainty.
- Specialized Engagement: Unlike horizontal platforms, it focuses on high-intent clinical queries and peer-validated medical insights.
Global Context: System Failures and Monopoly Risks
Dr. Prabhu provided a sobering comparison between India's emerging digital ecosystem and the established systems in the West.
- Western System Failures:
- United States: The system is widely perceived as failing due to the massive overhead and inefficiencies driven by the insurance-first model, which prioritizes payer-provider negotiations over patient outcomes.
- United Kingdom (NHS): While conceptually sound, the NHS is currently struggling with severe bottlenecks in access to doctors, with patients facing months-long waits for standard appointments and procedures.
- The Monopoly Risk: A recurring theme in the session was the caution regarding Mergers and Acquisitions (M&A) in the Indian private sector. While consolidation can drive efficiency, it also brings the risk of monopolies, which can stifle innovation, limit patient choice, and drive up costs in the long run.
The Rise of Medical Tourism
Amidst these global challenges, India's tertiary sector is emerging as a global leader in Medical Tourism. - Quality at Scale: By combining international-grade accreditation (JCI/NABH) with high-volume clinical expertise, Indian corporate hospitals provide outcomes comparable to the best in the West. - The Cost Arbitrage: India offers these world-class services at a fraction of the cost found in the US or Europe. This combination of "Top Quality" and "Low Cost" is positioning the country as the definitive global hub for complex medical procedures, further incentivized by the digital transparency brought by ABDM.
By triangulating across these three—Identity (ABHA), Verification (DigiLocker), and Discovery (ABDM)—the mission creates a "trust bridge" that ensures data is verified at the source and accessible at the point of care.
Bioinformatics & The CRO Revolution
- Digital Disruption: Dr. Prabhu detailed how the digitization of health data is fundamentally disrupting the multi-decade drug discovery lifecycle.
- Shrinking the 10-Year Window: Traditionally, bringing a drug to market is a 10-year journey. Through Bioinformatics and advanced data management, this window is being significantly compressed.
- Clinical Research Organizations (CROs): These organizations act as the execution arm for pharma companies, managing the complex 4-Phase Trial Lifecycle:
- Phase 1 & 2: Selecting populations and testing safety/efficacy.
- Phase 3 & 4: Post-marketing surveillance once the drug is in the wild.
- The Tech Stack: CROs now rely on a sophisticated stack of Clinical Trial Management (CTM), Regulatory Compliance, and Bio-statistics to ensure data integrity and structured reporting.
Navigating the Challenges of Implementation
Successful digital health transformation encounters several critical challenges, each requiring a dedicated strategic solution.
Critical Challenges & Solutions
 Figure: Managing clinical resistance through robust change management.
Figure: Managing clinical resistance through robust change management.
 Figure: Ensuring data integrity and operational continuity during migration.
Figure: Ensuring data integrity and operational continuity during migration.
 Figure: Strategic budget planning to prevent scope creep.
Figure: Strategic budget planning to prevent scope creep.
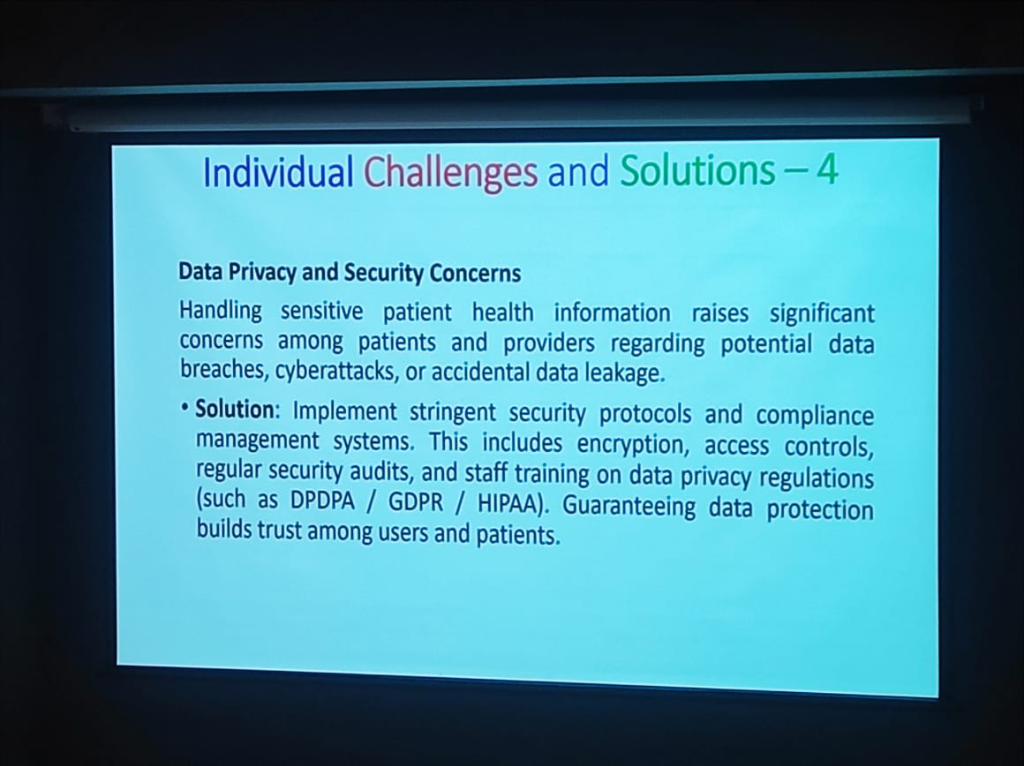 Figure: Compliance with global standards (ISO, DPDP) for trust.
Figure: Compliance with global standards (ISO, DPDP) for trust.
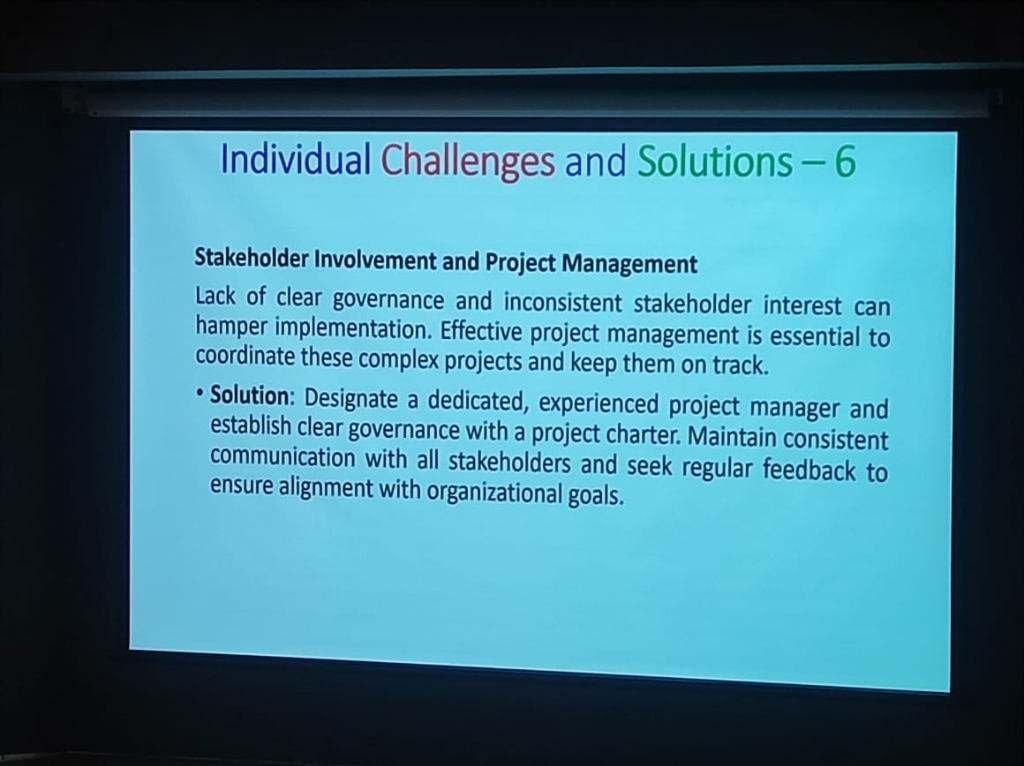 Figure: Coordinated project management for complex implementations.
Figure: Coordinated project management for complex implementations.
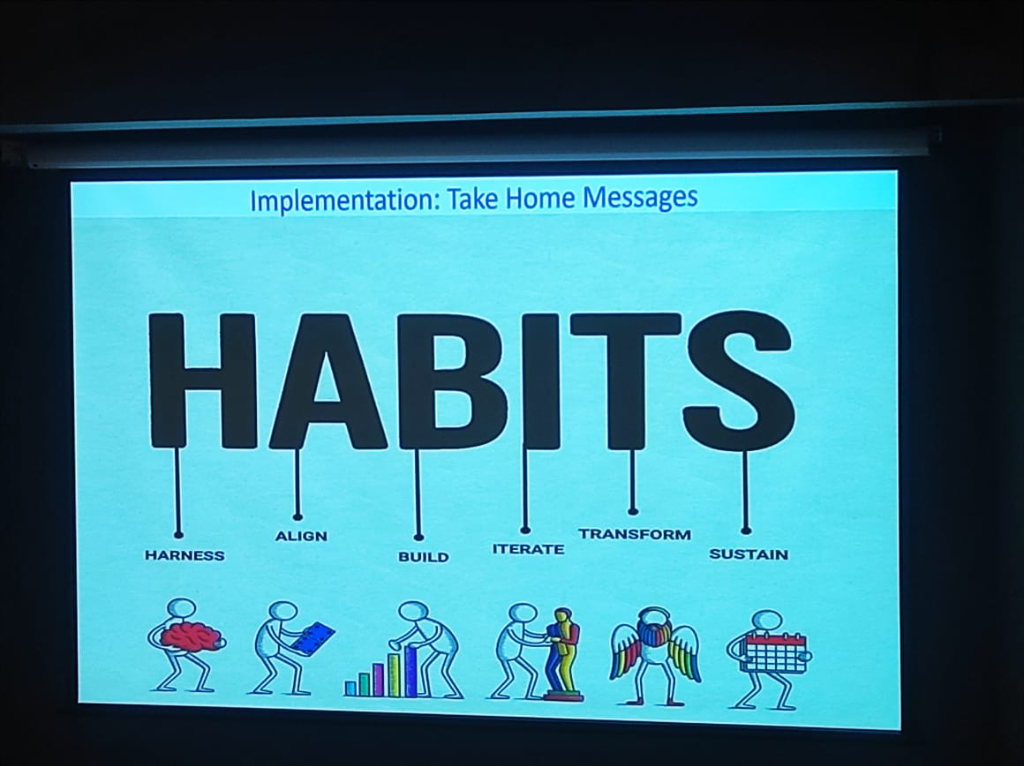
Key Takeaways: The HABITS Framework
The path to success is paved by building the right institutional HABITS: - Harness Align Build Iterate Transform Sustain.
Strategic Impact & Social Responsibility
KCDH’s mission extends beyond technical excellence to social impact and national policy.
Digital Equality & Public Goods
A critical discussion point was the "ROI Gap". Currently, digital transformation is primarily seen in Private Equity (PE) backed hospitals. To achieve Digital Equality and ensure health equity for marginalized populations, we must:
- Acknowledge Non-linear ROI: Digital health does not have a linear Return on Investment. Unlike hardware investments (CT or MRI scanners) where financial recovery is predictable, the ROI for HIS is measured through improved health outcomes and clinical quality—factors that are harder to quantify in short-term financial balance sheets.
- Equitable Access Strategies: Ensuring equitable access requires moving beyond "smartphone-only" models. Strategies must include Assisted Digital Interaction (via ASHAs or ANMs), Multi-lingual Interfaces, and Offline-first Architectures to reach populations with limited technological exposure or internet stability.
- Address the Intent Gap: Identifying and supporting hospitals that show the active intent to digitize, particularly in specialized areas like cancer care planning.
- Support the Koita Foundation: Ensuring funding and resources reach institutions with the highest potential for impact.
- Bridge Infrastructure Gaps: Addressing the critical maintenance and hardware needs in public hospitals to ensure continuous digital functionality.
National & Global Impact: From Care to Research
A major shift is recognizing the duality of medical data:
- Primary Usage: Direct clinical care using systems like EMR, EHR, and CDSS to improve immediate patient outcomes.
- Secondary Usage: Leveraging the same data for National Shared EHRs, clinical research, population health, and statistical analysis.
- Legacy Migration: Large institutions like Tata Memorial Hospital (TMH) face the immense challenge of migrating legacy EMRs (some with 50+ modules) into modern, AI-integrated systems.
- ABDM Integration: Aligning with the Ayushman Bharat Digital Mission to create India's health infrastructure backbone, leveraging FHIR to ensure that every clinical data point is discoverable and interoperable.
The Infrastructure Advantage: India’s Digital Readiness
As highlighted by Prof. Kshitij Jadhav, India is no longer just "digitizing" but is building a robust technological foundation for AI-native healthcare:
- Queryable Data vs. Scanned PDFs: A major shift is occurring in top health chains like Max Healthcare and Kokilaben Dhirubhai Ambani Hospital, where clinical data is no longer stored as static scanned PDFs, but as high-quality, Queryable Digital Data. This enables institutional research and real-time AI inference at scale.
- The GPU Backbone: India has invested substantially in hardware infrastructure, with a public-private partnership now providing over 30,000 GPUs dedicated to developing sovereign AI solutions. This massive compute capacity allows for the localized training of clinical models that account for Indian physiological and demographic diversity.
- The Skills Transfer Principle: AI expertise in India is highly transferable. The advanced engineering talent currently transforming sections like Financial Services, E-commerce, Agriculture (Agri), and Cyber Security is now applying the same rigorous Spark Analysis and deep learning techniques to the clinical space. The same "Skills Stack" that scales a global e-commerce platform is now being leveraged to scale patient-centered digital health.
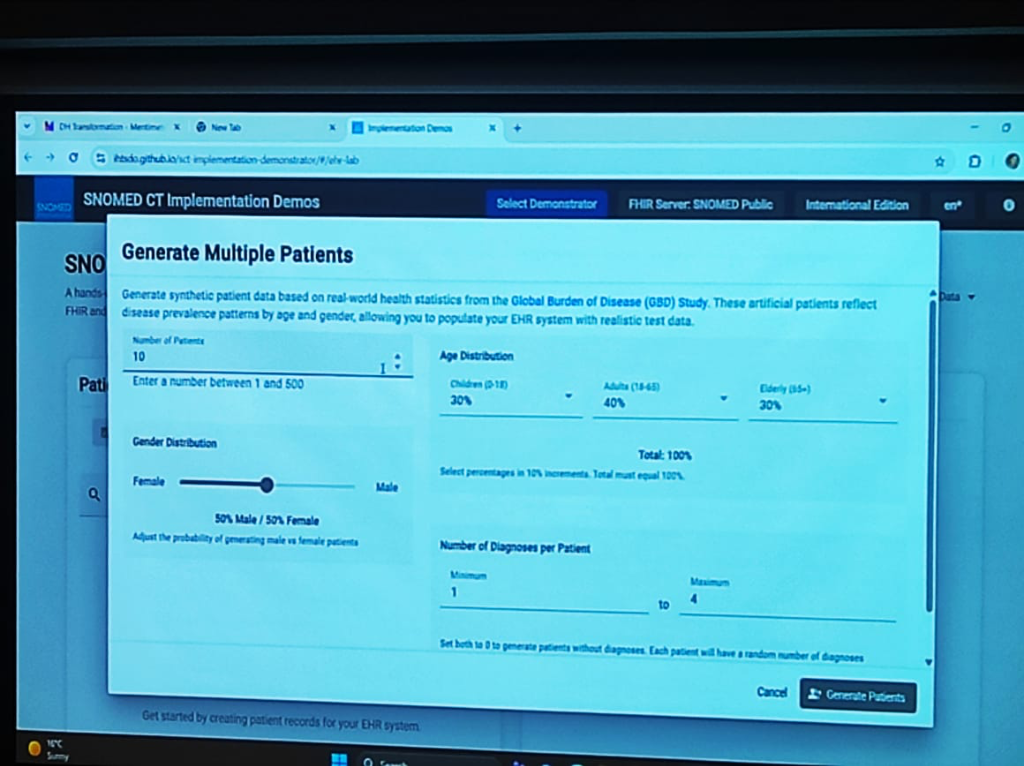
Demonstrating the Ecosystem in Action
The "Standard Trinity" and NRCeS frameworks aren't just theoretical; they are showcased through powerful live demonstrations that bring these concepts to life for clinicians and engineers alike.
Bridging Research and Practice
-
Synthetic Data Generation: Using the SNOMED CT Implementation Demonstrator, KCDH shows how to generate synthetic patient data based on real-world statistics from the Global Burden of Disease (GBD) Study. This allows for populating EHR systems with realistic test cases reflecting national disease prevalence patterns by age and gender.
-
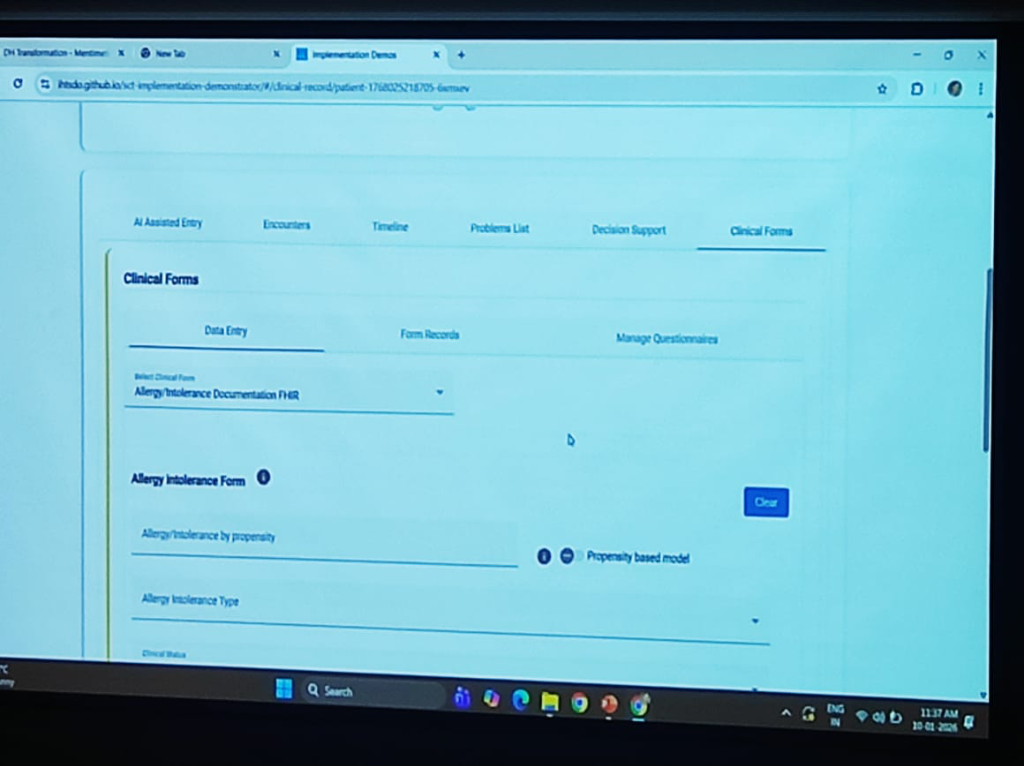
AI-Assisted Clinical Forms: The demo showcases FHIR-compliant Clinical Forms—such as Allergy and Intolerance documentation—enhanced with AI-Assisted Entry. This reduces the "key-in" friction for doctors by providing propensity-based models that predict likely clinical outcomes and decision support.
-
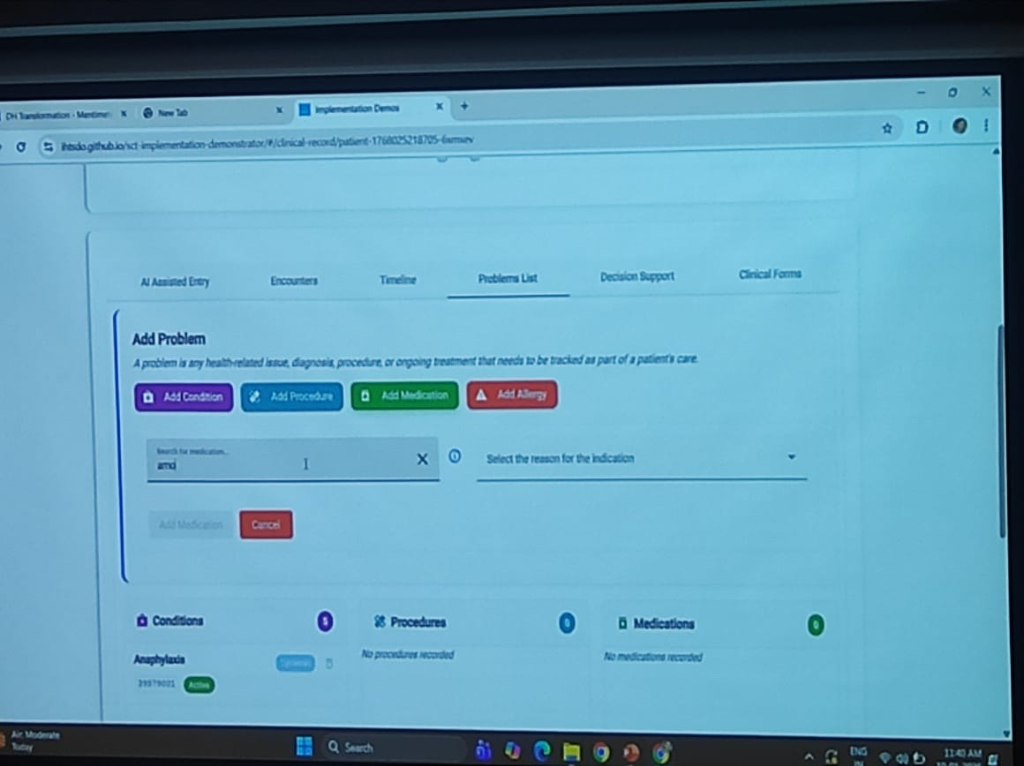
Clinical Decision Support (CDS) & Alert Generation: The ecosystem demonstrates real-time CDS Alert Generation. When a clinician adds a problem (e.g., Anaphylaxis) to the Problems List, the system automatically triggers alerts and decision support pathways based on standardized rules (e.g., contraindications or immediate care protocols). This transforms the EHR from a passive repository into an active participant in clinical safety.
-
Integrated Patient Timeline: Displays a unified problem list, timeline, and decision support—all powered by FHIR and SNOMED CT—providing a template for what a modern, interoperable HIS should look like.
-
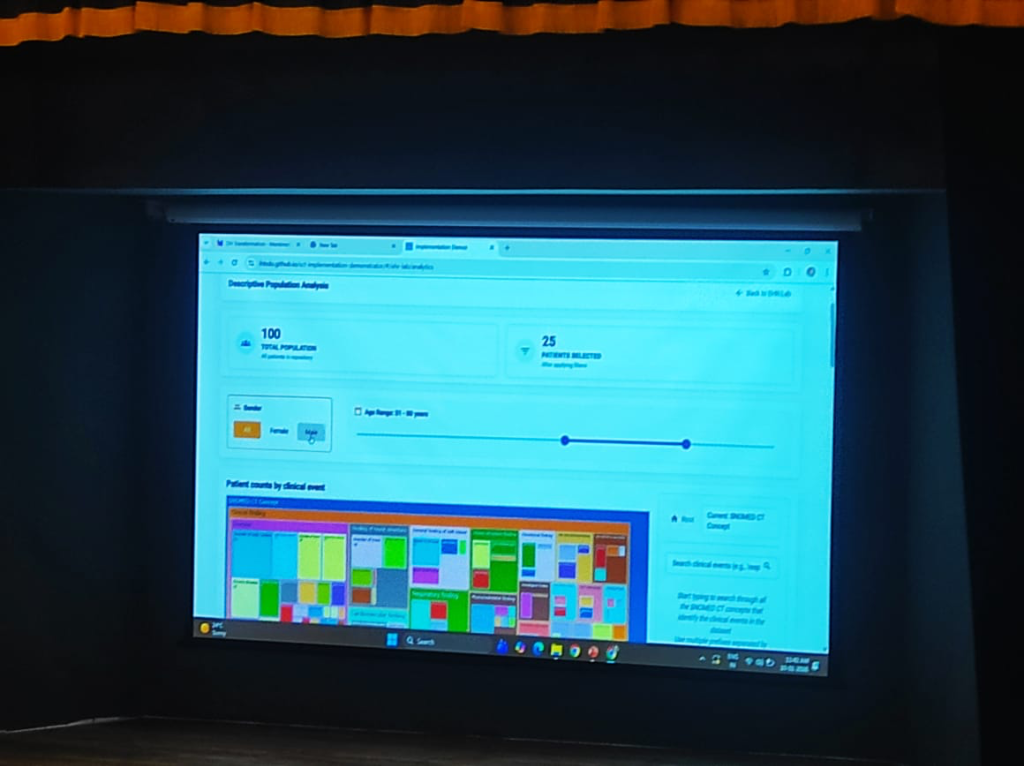
Descriptive Population Analysis: The power of standardized coding is best seen at the population level. By using SNOMED CT as the medical coding foundation, the system enables seamless Descriptive Population Analysis. Clinicians and researchers can filter and analyze patient counts by clinical events, age ranges, and gender distributions across the entire repository without any manual data cleaning.
The Way Forward: Building a Connected Ecosystem
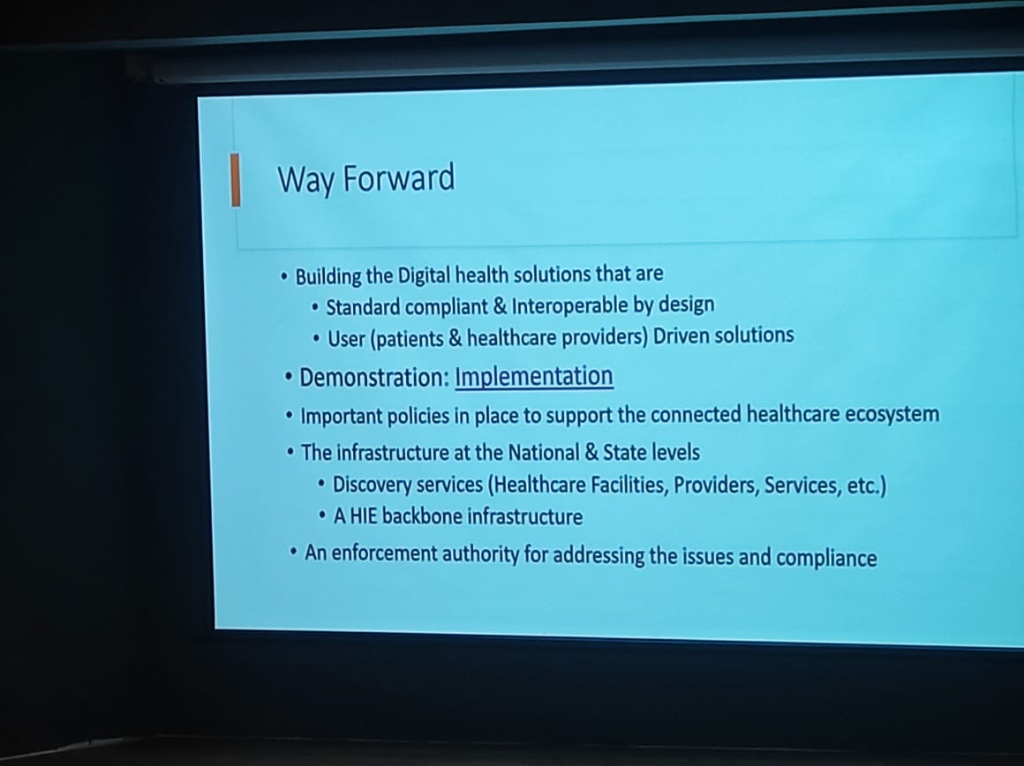
The path toward a fully digital healthcare system in India requires a transition from isolated projects to a cohesive national infrastructure.
Strategic Essentials
- Interoperable by Design: Future digital health solutions must be standard-compliant and interoperable from the ground up, rather than attempting to retro-fit integration later.
- User-Driven Solutions: Platforms must be designed with both patients and healthcare providers in mind, ensuring that the technology solves real-world clinical friction instead of adding to it.
- Evidence through Demonstration: Move from theoretical frameworks to demonstrable implementation that proves the value of digital health in real clinical settings.
Infrastructure & Governance
- National & State Level Infrastructure: Establishing robust Discovery Services to identify and catalog healthcare facilities, providers, and services at scale.
- The HIE Backbone: Strengthening the Health Information Exchange (HIE) backbone to facilitate seamless data flow across the country.
- Enforcement & Compliance: Establishing an enforcement authority to address compliance issues and ensure that stakeholders adhere to national health data standards.
Key Strategic Requirements (The Path Ahead)
The transformation of Indian digital health hinges on addressing several core strategic questions. These requirements serve as the benchmark for any institution seeking to achieve true clinical excellence and social impact.
- Rural Literacy: How can doctors in rural areas overcome digital literacy and infrastructure challenges?
- Equitable Access: What strategies can ensure equitable access to digital health tools for marginalized populations?
- AI vs. Judgment: How should clinicians balance AI decision support with clinical judgment and patient preferences?
- Professional Advocacy: What role can professional associations play in capacity building and advocacy for digital health?
- Global Adaptation: How can India’s digital public goods be adapted for global health equity and collaboration?
The Role of Professional Associations
Collective transformation requires more than just individual institutional effort. Professional Associations (such as NABH, DSCI, IMA, and specialty-specific bodies like IAP or API) play a pivotal role in:
- Capacity Building: Organizing cross-institutional training and knowledge-sharing workshops to bridge the digital literacy gap.
- Standard Advocacy: Lobbying for clinical-first standards and ensuring that regulatory mandates (like DPDP) are operationally feasible for front-line doctors.
- Peer Mentorship: Creating networks of "Digital Leaders" who can guide smaller clinics through the complexities of HIS/EMR adoption.
India's Digital Public Goods (DPGs)—specifically the ABDM framework and the NRCeS FHIR profiles—are not just for domestic use. They serve as a Global Blueprint for health equity.
- Adaptability for Global Equity: India's health stack is designed for scale and diversity, making it an ideal template for other developing nations seeking to build interoperable, patient-centric digital health infrastructures.
- Cross-Border Collaboration: By adopting universal standards, India facilitates global research collaboration, allowing for standardized comparative studies on disease burdens and treatment efficacy across diverse populations.
Implementation Roadmap: The Path to Accreditation
Successfully transitioning to a standard-driven institution requires a deliberate, phased approach. Healthcare leaders can follow this 10-step implementation journey:
- Leadership Commitment: Anchoring the transformation in institutional policy and board-level support.
- Digital Masterplan: Defining the long-term architectural and clinical objectives.
- Gap Assessment: Auditing existing systems and infrastructure against national standards.
- Policies & SOPs: Drafting digital clinical protocols and standard operating procedures.
- Software Alignment: Configuring EMR/HIS systems to meet standard specifications.
- Staff Training: Breaking the human barrier through hands-on learning and digital literacy programs.
- Pilot & Scale: Testing the standards in a controlled environment before a full institutional roll-out.
- Internal Audit: Verifying compliance and clinical data integrity internally.
- Accreditation: Moving toward formal recognition under the National Digital Health Standards.
- Continuous Improvement: Establishing an iterative cycle of quality audits and technology updates.
 Figure: The 10-step strategic roadmap for hospitals to achieve national digital health accreditation.
Figure: The 10-step strategic roadmap for hospitals to achieve national digital health accreditation.
Conclusion: A Call to Strategic Action
The digital transformation of Indian healthcare is not an IT upgrade; it is a clinical and organizational rebirth. The Koita Centre for Digital Health (KCDH) has demonstrated that the technical blocks—FHIR, SNOMED CT, ABCD—are ready. The question remains: Are the leaders ready?
Breaking the Silos: Quality, Clinical, IT
The most critical takeaway for any healthcare administrator is that these standards are the only tool capable of breaking institutional silos. National Standards (NABH) are inherently superior to proprietary Vendor Standards, which often create "walled gardens" that trap patient data. By adopting national standards, leaders bring together the Quality, Clinical, and IT teams under a single, unified mission: patient safety through data integrity.
The Iterative Approach
We urge healthcare leaders to avoid the "big bang" implementation fallacy. Instead, commit to a progressive, iterative approach.
- Understand the Standards: Move beyond jargon and grasp the operational value of semantic interoperability.
- Motivate Your Teams: Position standards not as a compliance burden, but as the clinical foundation for the next decade.
- Execute and Refine: Start with the "Minimum Data Set" and move incrementally toward total excellence.
Maintained by AlphaPebble Labs.